 Does stress reduce milk production?
Does stress reduce milk production?
Consider this scenario: You are late for an important appointment. You are just starting out the door when you discover baby poops through his last clean outfit and all over you, too! Your phone is buzzing in your purse and your hands are full with baby, diaper bag, and poop. That is a stressful moment, right? Every mom experiences high stress moments just like this.
Moms often hear that they should stay calm because feeling stressed will cause milk to “dry up”. The business of daily life, finances, relationship issues, illness, etc. are all common stressors moms face. Sometimes stress is sudden and ongoing such as in the case of natural disaster or war. The woman’s body is made to not only grow a baby, but also nourish and protect him once born. Moms can continue to breastfeed despite incredible circumstances.
Sometimes moms experience stress that is severe and intense, which can temporarily inhibit letdown. This is thought to be a protective mechanism. As one doctor put it so well, you wouldn’t want to be leaving a trail of milk behind if you were running from a tiger! Over a long period of time, it is possible for chronic stress to inhibit letdown often and long enough that milk production can be decreased. This is usually not the case, as breastfeeding releases hormones that helps mothers and babies both relax and have an easier time enduring stress, even under the worst of circumstances.
What can I do if I’m in a situation where I’m under ongoing, chronic stress and it is affecting my letdown?
Letdown can be triggered by associations, such as sights, smells, and emotions. Below are some tips for initiating letdown before and during breastfeeding or pumping. You can try any combination of these that makes sense to you.
- Find a location to feed your baby (or pump) where you feel very comfortable and safe. Choose a place that is free from intrusion and distraction.
- Make an effort to relax as much as possible before feeding or pumping. Listen to music, take a few cleansing breaths, pray, smell a relaxing scent, or do anything else that helps you feel at peace.
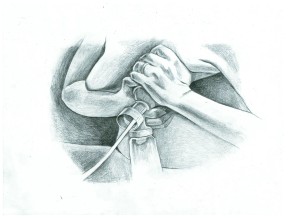
- Consider trying breast massage prior to nursing or pumping. It has been shown to assist with milk ejection and overall milk removal.
- Bend over at your waist so that your breasts dangle from your rib cage, and shimmy your shoulders (move them back and forth) so that your breasts shake. This movement helps loosen tension in your neck and shoulders and assists milk in moving forward in the breast.
- Consider using Reverse Pressure Softening (RPS) to promote letdown: “Steady stimulation of the nerves under the areola automatically triggers the milk ejection reflex, propelling milk forward in the breast, nearly always within 1-2 minutes or less.”–Jean Cotterman
- Enjoy the moment. If you are with your baby, smell his head and stroke his hair. If you’re away from your baby, smell a piece of his worn clothing and/or listen to his cries on a recording. Some moms like to watch videos of their baby cooing, crying, or breastfeeding on their phone. This creates an emotional connection, and can help promote milk release.
- Visualize milk spraying forth from your breasts like a waterfall or a rushing river. It sounds strange, but it often works!
- If you are with someone you trust and feel comfortable asking, have them rub your shoulders and apply pressure between your shoulder blades. This, too, can help trigger the release of oxytocin and assist in milk ejection.
- Drink water. Moms often sip water while nursing, so that alone may initiate letdown through what is known as conditioned response.
- If you’re pumping, the hands-on pumping technique can aid in milk ejection and help you maximize milk removal.
- Consider breastfeeding while bathing with your baby. This can help release tension in your muscles, and may help your milk flow freely.
- Between feedings, spend time in skin-to-skin contact with your baby. This will help you both relax, and aid in release of hormones associated with breastfeeding.
Breaking free from stress
- Talk to a counselor or traditional healer. Ask family and friends for support. Stress is often relieved by talking through your feelings and concerns, even if there isn’t a solution to your current problem.
- Contact your IBCLC, WIC PC, or volunteer breastfeeding counselor for continued support, including tips to manage stress as it relates to mothering and breastfeeding.
- Eat well and exercise. Eating nutrient-dense foods gives your body the necessary vitamins, minerals, and energy needed to overcome stress. Exercise is a well-known stress buster. Even a 30 minute walk around the block can lower blood pressure, ease tension, and clear your mind.
- Contact a medical or mental health professional if you’re experiencing ongoing, chronic stress. They can provide information for stress management, and evaluate for related issues like depression and anxiety.
- Consider talking to your doctor about taking a magnesium supplement. This mineral is often depleted during times of chronic stress, and some experts suggest that supplementation may help reduce stress-related symptoms.
Stress Resources:
Coping With Perinatal Stress and Depression by Cynthia Good Mojab, MS, LMHCA, IBCLC, RLC, CATSM
Mental Health Care for Postpartum Depression During Breastfeeding by Cynthia Good Mojab, MS, LMHCA, IBCLC, RLC, CATSM
American Heart Association: Four Ways to Deal With Stress
American Psychological Association: Coping with Stress and Anxiety
Working Moms and Stress Relief
Uppity Science Chick: The stress-lowering effects of breastfeeding (list of reference articles)
The Toxic Effects of Stress on American Indians
References:
Chen, D., Nommsen-Rivers, L., Dewey, K., & Lonnerdal, B. (1998). Stress During Labor and Delivery and Early Lactation Performance. Obstetrical & Gynecological Survey, 68(2), 81-82.
Dewey, K. (2001). Maternal and Fetal Stress Are Associated with Impaired Lactogenesis in Humans. The Journal of Nutrition, 133(11), 30125-30155.
Groer, M., Davis, M., & Hemphill, J. (2002). Postpartum Stress: Current Concepts and the Possible Protective Role of Breastfeeding. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 31(4), 411-417.
Heinrichs, M., Neumann, I., & Ehlert, U. (n.d.). Lactation and Stress: Protective Effects of Breast-feeding in Humans. Stress: The International Journal on the Biology of Stress, 195-203.
Lau, C. (2001). Effects of Stress on Lactation. Pediatric Clinics of North America, 48(1), 221-234.
Mezzacappa, E., & Katkin, E. (2002). Breast-feeding is associated with reduced perceived stress and negative mood in mothers. Health Psychology, 21(2), 187-193.
© Jolie Black Bear 2015